Our Perpetual Government-Sponsored Food Fight
And the quacking solution.
-
Tools:
Anybody who follows nutrition advice in the popular press can be forgiven for thinking that dietary advice is unreliable and uncertain. We've heard that caffeine is bad for the heart, then that it's good for the heart, then that it's bad in certain cases. Who knows?
For centuries, activists pontificated about the Evils of Drink. Then it turned out that red wine consumed in moderation is good for the heart. Then it turns out that you can get the same effect by drinking the right kinds of grape juice - or maybe you can't. Who knows?
The reason for all the confusion lies where the economics and profits of producing and selling food products meet government regulation. Although the stated goals of the agencies which regulate food and drugs are commendable, the objectives of protecting public health have become entangled in politics as with all government agencies.
The result has been confusion for the people who consume drugs, food, and food supplements and great wealth for companies who manage to manipulate the political processes so that that our laws favor their products.
The amounts of money involved are huge; food supplements alone are a multi-billion dollar market which produce lots of campaign contributions, so there's no chance of taking politics out of food regulation. This article explains the basic forces which drive our ongoing food fight, and ends with a modest suggestion of a way we could have a bit more medical research done and save the lives of some desperate people without excessively threatening our current bureaucratic empires which oversee food and drugs.
Where It All Started
The US Department of Agriculture was created in 1862 and given the task of a) insuring a reliable food supply and b) spreading useful information on subjects concerning agriculture. The agency interpreted part (a) as their mandate charging them with promoting agricultural interests and part (b) as requiring them to spread information about the effect of diet on health. The USDA started studying the relationship between agriculture and nutrition in 1890.
At the time, vitamins had not been isolated and the dietary causes of scurvy, beriberi, pellagra, goiter, and other diseases of malnutrition were just beginning to be understood. In the absence of concrete information, it made sense for the department to encourage people to eat as wide a variety of foods as possible.
The resulting "eat more of everything" message coincided with the interests of food producers. Any food could be assumed to contain some nutrients; producers were happy to promote their products as contributing to a healthful, high-variety diet.
Since then, though, increased scientific knowledge has resulted in a pitched battle between regulators, products, and consumers, because of the ever-increasing complexity of food and drug regulation. The more we learn about medicine and nutrition, the worse the regulatory mess becomes.
The Big Food Fight
The root cause of the upcoming food fight between producers, consumers, and government regulators was documented by W. O. Atwater, the first USDA director of research, in 1894. He confirmed "the general impression of hygienists that our diet is one-sided and that we eat too much ... fat, starch, and sugar. This is due partly to our large consumption of sugar and partly to our use of such large quantities of fat meats. ... How much harm is done to health by our one-sided and excessive diet no one can say. Physicians say that it is very great." (Atwater, WO, Foods: Nutritive Value and Cost, Washington DC:USDA 1894 p 25)
Atwater went on to recommend a diet where 15% of the calories came from protein, 33% from fat, and 52% from carbohydrates. His recommendations are surprisingly close to modern advice. Most advisers of his day and for many years thereafter followed the "eat more of everything" approach, helped by the Great Depression and World War 2 where most people didn't have enough of anything and would gladly take whatever they could get.
"Eat more of everything" came under stress in the 1970's. By that time, it was recognized that consuming too much fat, cholesterol, and sugar was harmful to health. It was also seen that Americans were beginning to get fatter because they ate more calories than they burned through physical activity.
At the same time, the tremendous increase in national wealth of the 1950s and 60s had resulted in a world where almost all Americans could easily afford as much food of whatever sort they wished as they could physically pack down.
There was an inherent conflict between the USDA's mission to promote farming interests and their mission to give sound nutrition advice, of course. Food producers were convinced that any message suggesting "eat less" would stigmatize their foods as "bad" and have negative impact on sales, whereas consumer advocates were enraged that the USDA food recommendations continued with the "eat more" mentality.
During the 1980's, changes in the recommendations were made to accommodate the food industry's fears. For example, "avoid too much" became "choose a diet low in" and "choose lean meat" became "have two or three servings of meat." The guidelines tried to avoid classifying foods as "bad" by referring to substances which were harmful in excess such as salt and fat but not referring to specific foods which contained them.
When the 1991 edition of the USDA's Food Pyramid was about to be published, the National Cattlemen's Association claimed that the Pyramid would cause people to eat less beef and that beef should not be placed so close to fats and sugars in the diagram; they were worried about guilt by association.
The Pyramid was delayed and national news media noticed how food producers were influencing the USDA. This phenomenon went back 100 years but had not received national publicity before.
A few changes were made in the wording of the Pyramid and the new version was released a year later.
In the same vein, the USDA forbade a meatpacker to test its cattle for mad cow disease. The meatpacker had intended to privately test all its cattle; USDA tests only 1 percent of cattle. Arguing that full testing would cause the public to question meat safety, USDA moved to stop it.
The Bigger Health Claim Fight
The wording of a government pamphlet which tried to explain how to choose foods for nutritional benefit caused heated controversy as food producers tried to avoid having the government urge people to eat less of their products.
The level of popular interest in the Pyramid controversy showed that people had become interested in diet and health. Manufacturers began to realize that they could make money if they could advertise foods or other products as "good" or "healthy." The desire of food producers to make health claims for their wares, though, brought the FDA into the fight.
The Federal Drug Administration was chartered to ban medical products which were either unsafe or ineffective. As soon as vitamins were discovered, of course, companies started marketing them as food supplements. Marketers focused on middle-class, educated women who were unlikely to actually suffer from vitamin deficiencies, but could afford to worry that they might. Marketing was so successful that vitamin sales rose from $32 million in 1932 to $82 million in 1935, during the Great Depression.
The FDA decided that vitamin supplements were drugs which fell under its regulatory umbrella. Most FDA staff believed that most people received adequate amounts of vitamins in their diet and had no need of supplements. The FDA took the position that scientific proof of a benefit was needed before a vitamin or any other nutritional supplement could be marketed on the basis of medical effectiveness and that people shouldn't take vitamins unless a physician had determined that they suffered from a deficiency.
The manufacturers did not want their potions regulated as prescription drugs and argued that if a customer believed that he or she benefited from a supplement, the American tradition of freedom of choice meant that the customer ought to be free to buy and consume the product. As a glance at Wal-Mart's drug section clearly shows, this point of view eventually carried the day.
All-Bran and the National Cancer Institute
The first major blow against the FDA's policy of regulating health claims came from Kellogg. Kellogg worked closely with the National Cancer Institute, which, like the FDA, is part of the U.S. Department of Health and Human Services. In 1984, Kellogg put this message on its All-Bran cereals:
The National Cancer Institute believes eating the right foods may reduce your risk of cancer. Here are their recommendations: Eat high-fiber foods. A growing body of evidence says high-fiber foods are important to good health. That's why a healthy diet includes high-fiber foods like bran cereals.
The NCI believed that Kellogg's statement was a perfectly reasonable message about health, but Kellogg's use of the NCI and making health claims in an advertising campaign surprised the FDA. The FDA realized that if Kellogg was not stopped, health claims would slip from their regulatory grasp.
Their objections were overruled when the Federal Trade Commission supported the NCI by pointing out the public benefits of spreading information about dietary health. All-Bran increased its market share 47% in six months, despite tasting and looking more akin to twigs and straw than to edible food.
The food industry realized that health claims sold products even if they tasted hideous and looked appalling! The battle was on.
Vitamins were already a big business and the FDA had been trying to regulate them for years. In 1993, the FDA broadened its definition of supplements from vitamins and minerals to include herbals, botanicals, and most other products sold in health food stores.
The FDA had always advocated a "scientific" approach to selling vitamins and minerals. The FDA wanted the manufacturers to demonstrate that their products were both effective and safe before selling them, but this position would have had the same effect as a complete ban since it can cost as much as a billion dollars to shepherd a drug all the way through the approvals process.
Traditional herbal products cannot be patented because they're found in nature; there would be no way for a manufacturer to recoup the immense cost of the sort of clinical trials the FDA demanded for drugs. Not only that, it's essentially impossible to identify the vitamin and mineral content of foods people eat.
Even if people were able to report accurately on what they eat, it's difficult or impossible to determine what nutrients have been consumed. The USDA publishes data on the nutrition content of foods, but these data become outdated as new food products are introduced or recipes change. Thus, it's pretty much impossible to demonstrate that a) the user was not getting enough of whatever is being tested without taking the supplement and b) that there was benefit from taking the supplement.
Food supplement companies realized that being treated as drug manufacturers would put them out of business, so they organized lobbying efforts to persuade Congress to limit the FDA's ability to police their marketing claims. They organized letter-writing campaigns, put up posters in health food stores, and exercised their constitutional right to petition their elected representatives for redress of grievances.
Their lobbying efforts were helped immensely by the fact that people were beginning to demand the right to decide their own medical treatments. Many supplement users believed that the FDA was a pawn of major pharmaceutical firms and was trying to ban food supplements to force sick people to impoverish themselves by buying from big pharma.
As a result, the law was changed in 1994 to permit most of the health claims which the FDA had questioned. Many court cases followed which further limited the FDA's ability to limit marketing claims. At the moment, food supplement manufacturers do not have to prove the efficacy of their products and aren't required to ensure that the ingredients in the product are as claimed on the label.
The market results were immediately evident. In the first year after the 1994 law deregulated marketing, supplement sales went from $4 billion to $15 billion. Food companies started looking for ways to add herbals to their foods so that they could make similar claims, and drug companies considered selling their products as over-the-counter health foods.
Cholestin and Tamoxifen
Cholestin is a product made of milled rice fermented with red yeast. This mixture has been used in Asia as a health food for thousands of years.
Investigation showed that the capsules had at least nine compounds which lowered blood cholesterol. One of them was virtually identical to Lovastatin, a drug which had been previously approved through the standard high-cost regimen of clinical trials.
The FDA sought to treat Cholestin as a drug but was overruled by the courts. Cholestin can be sold much more cheaply than Lovastatin because the manufacturer is not subject to the FDA's regulations and need not recoup the cost of clinical trials. A user can buy a month's supply of Cholestin for about $30 as opposed to the $120-350 which prescription Lovastatin would cost.
The FDA defends its regulations as necessary to protect public health, of course, but there would seem to be room for a degree of relaxation given the cost differential between Cholestin and Lovastatin. However, only one of these, despite being chemically the same, is marketed energetically to doctors. Which do you suppose gets used by more patients in need, if they have health insurance?
To be fair, the science of nutrition is extremely complex. Most natural foods contain many different ingredients which have nutritive value and interact in poorly-understood ways whereas drugs contain very few active ingredients and generally only one. We're learning that prescription drugs interact in subtle and often complex ways; the interaction between nutrients is at least as subtle and far more complex because there are many more active compounds involved.
This renders the FDA clinical-trial approach unsuitable for herbal medicines, just as it doesn't work for individualized treatments based on a patient's genetics.
Not only that, medical folk are beginning to realize that a patient's genetic makeup affects whether FDA-approved drugs work or not. The New York Times wrote "Experts say that most drugs work for only about half the people who take them" and reported that tamoxifen, a drug which had passed clinical trials for helping prevent recurrence of breast cancer, works only on patients with the appropriate genetic makeup.
In 2003, more than 25 years after tamoxifen was introduced, researchers led by Dr. David A. Flockhart at Indiana University School of Medicine figured out that the body coverts tamoxifen into another substance called endoxifen. It is endoxifen that actually exerts the cancer-fighting effect. The conversion is done by an enzyme in the body called CYP2D6, or 2D6 for short. [emphasis added]
But variations in people's 2D6 genes mean the enzymes have different levels of activity. Up to 7 percent of people, depending on their ethnic group, have an inactive enzyme, Dr. Flockhart said, while another 20 to 40 percent have an only modestly active enzyme. [emphasis added]
Tamoxifen was approved after the usual full-court-press clinical trial regimen. Twenty-five years later, researchers find that 7% of patients don't benefit from it at all and 20-40% benefit only a little. This suggests that patients who actually do benefit gain a lot; the drug was found to be effective even though the study probably included people who couldn't benefit one bit due to their inappropriate genetic makeup.
In spite of following the standard multi-million dollar drug trial protocol, nobody had a clue how tamoxifen actually worked even though the drug merchant had studied the drug extensively before even starting the clinical trials. Knowing that a drug works, at least in some people, isn't quite the same as knowing how or why it works.
It's far more difficult to tease out the effects of herbal medicines because plants have so many ingredients which interact with whatever nutrients are found in food. Not only that, the actual content of a specific dose of an herb depends on the soil where it was grown, the particular strain of seed, how it was watered and fertilized, when it was harvested, and a host of other environmental factors.
In addition, the lack of patent protection means that there's no way for whomever pays for the testing to get their money back. Requiring scientific proof of effectiveness would effectively ban almost all food supplements, so the industry lobbied to force the FDA to leave them alone.
This ended up with a "pretty much anything goes" atmosphere which is good for business if not for health.
Tryptophan
In 1989, at least 1,500 people who took tryptophan, an amino acid which is found in all food proteins, became seriously ill and about 40 died. The problem seemed to be related to taking the supplement (Roufs, JB. Review of L-tryptophan and eosinophilia-myalgia syndrome, Journal of the American Dietary Association 1992 pp 844-850).
The FDA tends to ban a drug which causes any fatalities regardless of whatever benefit it may bestow, and banned sales of tryptophan in 1991. It was soon found that the fatalities had been caused by a contaminated batch from a single manufacturer, but even after the problem was found and corrected, the FDA continued to assert that tryptophan was unsafe.
After much political argy-bargy, tryptophan was made available in its original form in 2001. The fact that it took a decade to undo an unjustified ban on a popular supplement did the FDA's credibility no good. People who believed they had benefited from tryptophan resented having to buy expensive drugs and suspected that the FDA was a marketing ally of big pharma.
People who believe that the FDA is needlessly delaying the release of drugs that could save their lives, on the other hand, think the FDA is a collection of hidebound bureaucrats who don't mind killing people and wasting precious drug research funds through obfuscation and inaction. Their point of view is reflected in the article "The FDA Is Killing Chron's Patients" which was published on p A9 of the Dec. 30 Wall Street Journal.
The Journal pointed out that the US Supreme Court has decided that the 5th amendment prohibition of depriving a person of life or liberty does not mean that patients should be permitted to take drugs of which the FDA disapproves. Those who regard this decision as a personal death sentence beg to differ and are making their views known in Washington insofar as their resources permit.
From the first, the FDA fought making supplement labels less rigorous than drug labels because if they cut food supplements any slack, drug companies would go to court to win the same privileges. When the FDA wouldn't back down, supplement partisans got a law passed to forbid the FDA to impose any labeling requirements for food supplements at all.
Having waged total war and won total victory, the supplement crowd is in no mood to compromise; we can expect to see more advertisements such as this one for water-stirring equipment with special minerals embedded in plastic to enhance the water's effectiveness in the body.
And The Fight Plays On
It makes no sense to have both the "promote agriculture" function and the "promote healthy diets" function in the same government agency because of the inherent and irresolvable conflicts between the two objectives; there's simply no way to reconcile "eat more" which pleases agribusiness and "eat less" which promotes better health.
The legislative committees that oversee the USDA are not interested in moving the dietary function to a different agency, however, because that agency would be overseen by a different committee. Losing influence over nutrition would reduce campaign contributions to members of the agriculture committees; they're nearly as enthusiastic about that prospect as the cattlemen are about government advising everyone to "eat less beef."
It's possible, of course, that having those conflicting functions in the same committee might cause campaign contributions to cancel each other out. We're reminded of a court transcript from the early days of the American West where the judge opened the trial by saying, "The court has in hand $10,000 from the plaintiff and $5,000 from the defendant. The court will return $5,000 to the plaintiff and try the case on its merits." Except that politician seldom return campaign contributions, this may be what's happening.
There are a number of conclusions we can draw:
- You can't believe anything you read about any health food product because marketing always trumps scientific accuracy and because actually verifying marketing claims is too expensive for non-patentable compounds. If the product works for you, however, it doesn't matter whether it really works or whether you just believe it works so long as it seems to work. Belief trumps science when it comes to health.
- Diet supplements may confer benefits - it's conceded that Cholestin generally reduces blood cholesterol - but nobody can afford to research exactly how the nine active ingredients interact in different people.
- The price difference between highly-regulated Lovastatin and unregulated Cholestin suggests that there should be some room for relaxing some of the more costly FDA regulations. Bureaucracies give up regulatory turf about as eagerly as food sellers give up market share, so this probably won't happen without another multi-year battle.
- The legislative process responds to monetary and political pressures; it's not particularly good at fact-finding because money speaks louder than truth.
- We've found all the simple, obvious nutrition requirements. Vitamin C deficiency causes scurvy in just about everyone, iodine deficiency causes goiter, etc. These substances were so essential to health that they were a lot easier to figure out than whether, say, zinc, copper, magnesium, or a zillion other compounds sold as nutraceuticals are actually needed and if so, how much and by whom. Our technology simply isn't good enough to prove whether these substances help or hinder health; the controversy will continue.
- There might be room for mechanisms for a) verifying that what's in the bottle matches the label and b) identifying dangerous compounds so that they can carry warnings, but there's no trust on either side to work out how to do that fairly.
- The billions and billions of dollars involved are sufficient to fuel the food fight for a long time to come.
The point is that decisions about what government and industry are allowed to say about nutrition are going to continue to be made as part of the money- and power-driven political process. As with all matters medical, it pays for each individual to learn as much as possible about whatever medicines and food supplements may be involved in a particular condition and become as knowledgeable as possible about medical treatment.
Matters of your health are far too important to be left to government.
That being the case, why do we allow the government to control whom you're allowed to consult for medical advice?
The Solution - License Quackery
We could relieve the current licensing dilemma by setting up a system for licensing quacks. Dictionary.com defines "quack" as "a fraudulent or ignorant pretender to medical skill."
Much of the impetus behind the legislation that gave the Federal Drug Administration control of drug sales in the United States was that so many "medical" potions were being sold which were either ineffective or downright dangerous.
In the early days, it was possible to run experiments to verify that a new drug was both safe and effective, but as we found all the easy drugs, the process has gotten more and more expensive and more and more people die waiting for drugs to be approved. Not only that, we're finding that individual genetic makeup has a lot to do with how each person reacts to drugs; this invalidates the FDA's traditional methodology of treating people as statistically equivalent.
Many fans of herbal food supplements think that if a chemical comes from a plant it's somehow "natural" and therefore less likely to do harm than a "drug" made in a chemical plant. That's silly - a great many medicines were discovered when drug companies analyzed plants to find "active ingredients" that had medical effects. A chemical is a chemical regardless of whether it comes from a plant that grows in the ground or a plant in an industrial neighborhood, pun intended.
One way to break the log jam and strike a blow for freedom at the same time would be to decide that the 5th amendment does allow any dying individual to pursue happiness by taking any substance at all if they've exhausted conventional treatments. Such a person could go to a licensed quack and take any treatment they desired, subject to the following rules:
- There's no legal liability whatsoever for anything a licensed quack does. Licensing means they've signed the National Quack Register and agreed to keep records of whatever they do.
- The quack can charge whatever the patient is willing to pay.
- The patient donates a blood sample before starting treatment so that any interesting genetic peculiarities can be explored later.
- The quack maintains complete records of every treatment administered to the patient to facilitate lessons learned.
- The quack's won-loss record is posted on the quack's web site.
The idea is that if someone's going to die, they have the right to do anything they like which might help them avoid death provided we can all learn from it. Doctors will protest because quackery would put a dent in their lucrative monopoly, but do we as a society really have the right to tell a person who's dying that they can't take laetrile? Or that they can't have St. John's Wort? Or anything else they can afford?
Who knows? If a quack cured a number of patients, we'd have medical data we'd not otherwise have, and more might be cured. Setting up a licensing mechanism for quacks would give the bureaucracy something to do and reduce the sting of their not being able to regulate what quacks do.
There are historical precedents for medical advances coming from outside the profession. Obstetrical forceps were invented by members of the Chamberlen family who kept them a closely-guarded trade secret for about 150 years. Their rate of childbirth complications was noticeably lower than their competitors; they profited mightily from keeping their invention secret, which was good for them, but keeping the secret to themselves was not so good for womankind at large.
We've written how unconventional medical treatments are being forced offshore due to overly stringent regulations; it would be beneficial to formulate some mechanism for experimenting with unconventional treatments in extreme cases.
Let's hear it for quackery!
-
Tools:
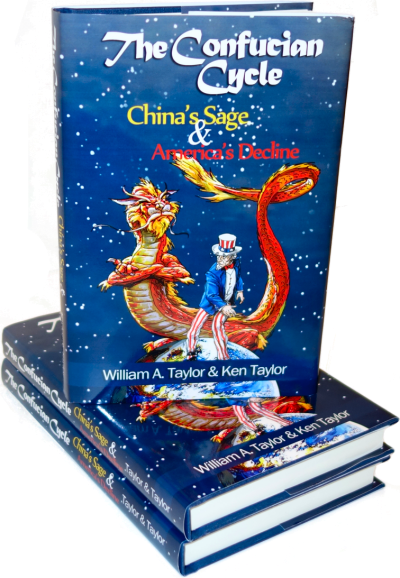
What does Chinese history have to teach America that Mr. Trump's cabinet doesn't know?

That should be the benefit of getting the FDA to approve your drug/supplement. That and, of course, the ability to put FDA approved on your label. Who knows how much that might lower drug costs. After all companies don't only have to recoup the cost of FDA approval but also have to make enough money for the inevitable lawsuits that will come at them.
MONTHS TO LIVE
Fighting for a Last Chance at Life
By AMY HARMON
A Virginia family's campaign for access to an unproven drug highlights the challenges many terminally ill patients face in the search for treatment.
http://www.nytimes.com/2009/05/17/health/policy/17untested.html
Big Food vs. Big Insurance
By MICHAEL POLLAN
The American way of eating has become the elephant in the room in the debate over health care.
http://www.nytimes.com/2009/09/10/opinion/10pollan.html
http://www.slate.com/id/2229194/
Ad Rules Stall, Keeping Cereal a Cartoon Staple
By WILLIAM NEUMAN
An effort to forge tougher advertising standards that favor healthful products has hit divisions among regulators.
http://www.nytimes.com/2010/07/24/business/media/24food.html?th&emc=th
Lucky Charms. Froot Loops. Cocoa Pebbles. A ConAgra frozen dinner with corn dog and fries. McDonald's Happy Meals.
These foods might make a nutritionist cringe, but all of them have been identified by food companies as healthy choices they can advertise to children under a three-year-old initiative by the food industry to fight childhood obesity.
Now a hard-nosed effort by the federal government to forge tougher advertising standards that favor more healthful products has become stalled amid industry opposition and deep divisions among regulators.
A report to Congress from several federal agencies - expected to include strict nutritional definitions for the sorts of foods that could be advertised to children - is overdue, and officials say it could be months before it is ready. Some advocates fear the delay could result in the measure being stripped of its toughest provisions.
"All of a sudden everything is dead in the water," said Dale Kunkel, a communications professor at the University of Arizona who is an expert on children's advertising. "I have heard no arguments to slow this down other than that the industry doesn't like it."
Among the requirements under consideration and included in a preliminary proposal by the agencies: Cereals could have only eight grams of sugar per serving, far less than many cereals that are heavily advertised to children (Lucky Charms and Cocoa Pebbles have 11 grams and Froot Loops has 12). The level for saturated fats would be set so low it would exclude peanut butter. And to qualify for advertising, all foods would have to contain significant amounts of wholesome ingredients like whole grains, low-fat milk, fruits or vegetables.
Critics have long complained that standards used by food manufacturers to designate healthy foods suitable for advertising to children are flawed, with ads for foods high in calories, fat, sugar and salt remaining a prominent part of the Saturday morning ritual on television. The Obama administration, as part of its campaign against childhood obesity, has also called on food companies to do more to ensure that advertising aimed at children is for healthier products.
The federal involvement took a step forward last year when Congress ordered the Federal Trade Commission, the Food and Drug Administration, the Agriculture Department and the Centers for Disease Control and Prevention to recommend standards for children's food advertising.
The food fight goes on at great expense.